States that provide a mixed model (with the exception of three states):
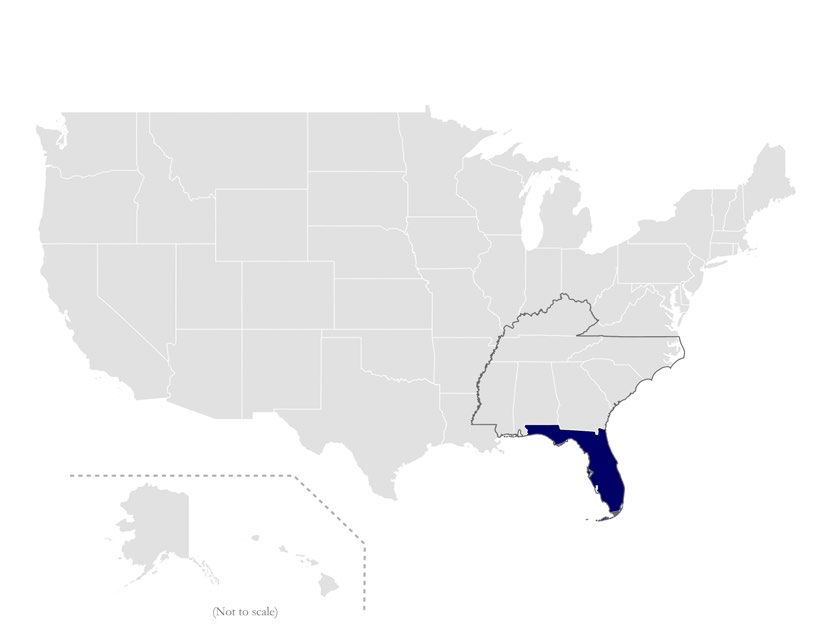
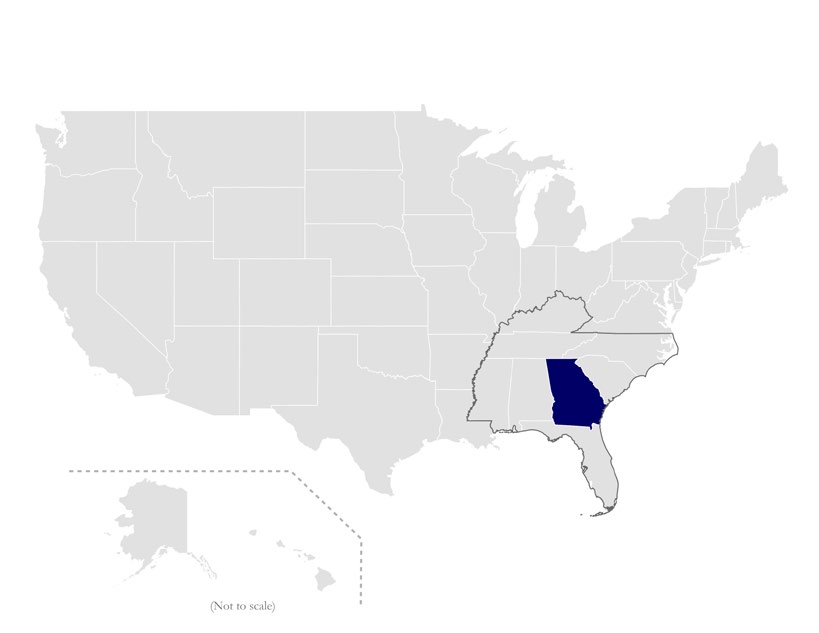
- Provide the vast majority of NEMT for Medicaid recipients through MCOs (see Table 1 and Figure 1)
- For the small number of Medicaid recipients that opt-out of an MCO, NEMT is provided through the state either as directly operated service or through a statewide broker.
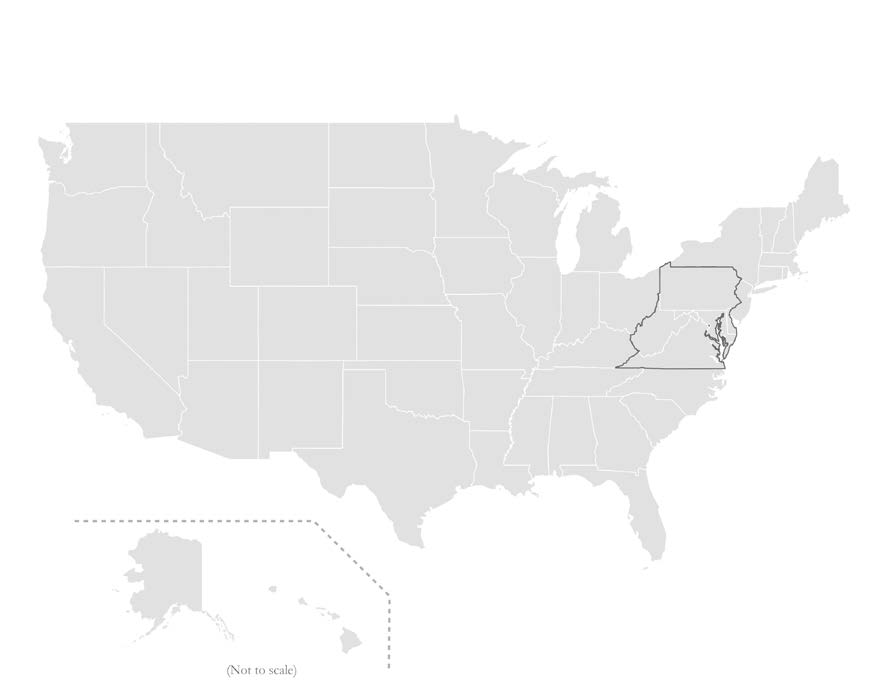
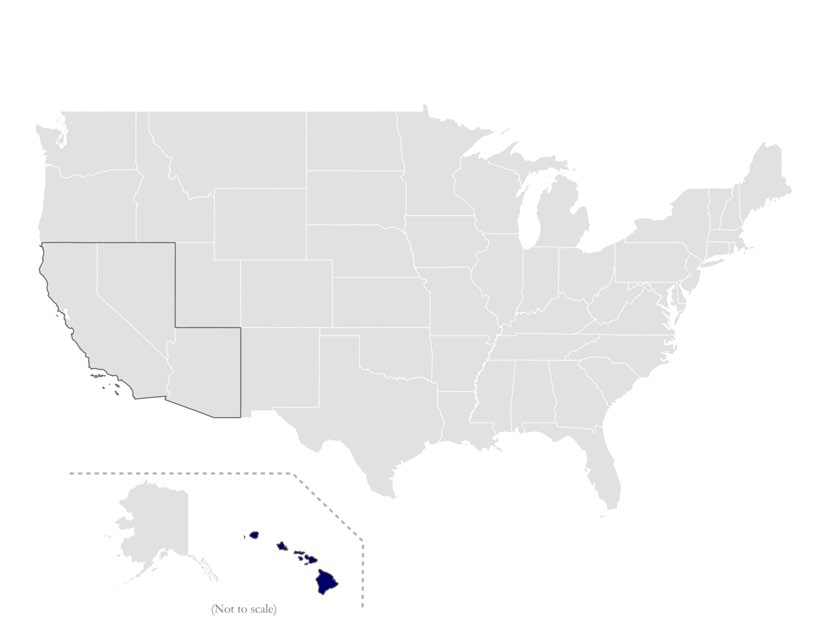
The three states that are the exception are Colorado, Michigan, and Pennsylvania that operate a mixed model where the state contracts with a regional transportation broker to provide NEMT around a major metropolitan area, and the remainder of the state is provided through state as a directly operated service.